背景
2019 冠状病毒病(COVID-19)是由 SARS-CoV-2(COVID-19病毒)引起的呼吸道感染。COVID-19病毒主要通过密切的身体接触和呼吸道飞沫传播,而在产生气溶胶的医疗程序中也可能通过空气传播\在本文发布之时,现有研究中尚未确定OVID-19病毒的传播与受污染的环境表面有关。但是,本临时指导文件的依据是卫生保健机构中存在表面污染的证据2,而且以往的经验表明表面污染与其它冠状病毒随后的感染传播相关。因此,本指导文件旨在减少污染物在卫生保健机构3和非卫生保健场所中COVID-19的传播方面可能发挥的任何作用4。
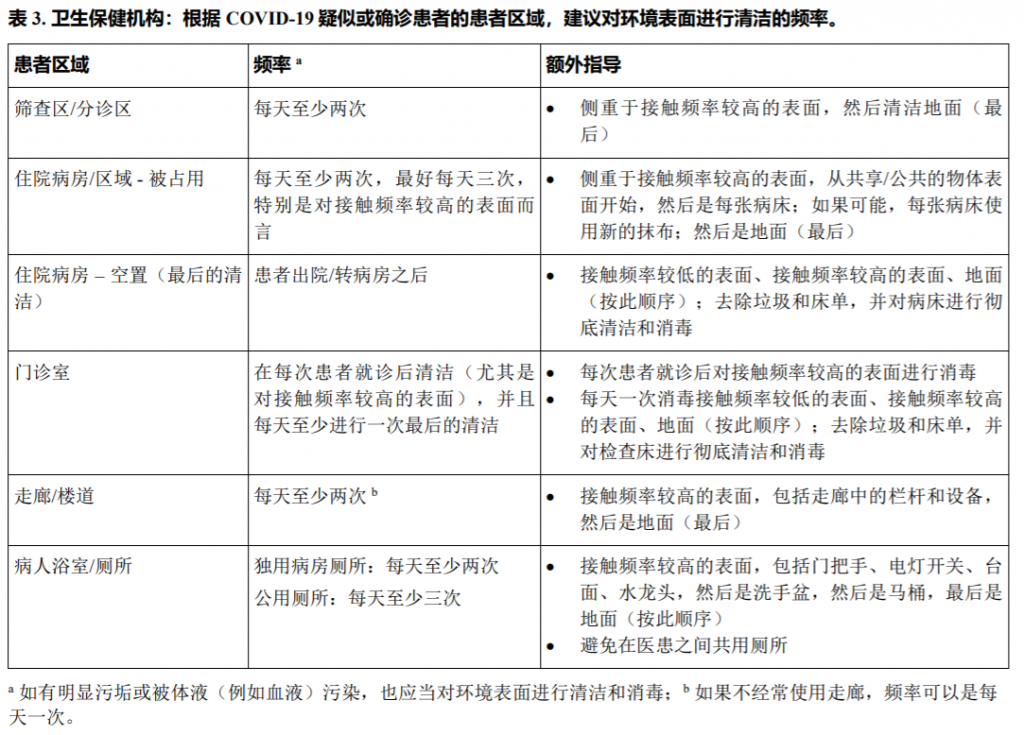
卫生保健机构中的环境表面包括病房和卫生间内外的家具及其它固定物体,例如桌子、椅子、墙壁、电灯开关和计算机外围设备、电子设备、水槽、马桶,以及非关键性医疗设备的表面,例如血压袖带、听诊器、轮椅和恒温箱5。在非卫生保健场所中,环境表面包括水槽和马桶、电子设备(触摸屏和控件)、家具及其它固定物体,例如台面、楼梯栏杆、地面和墙壁。
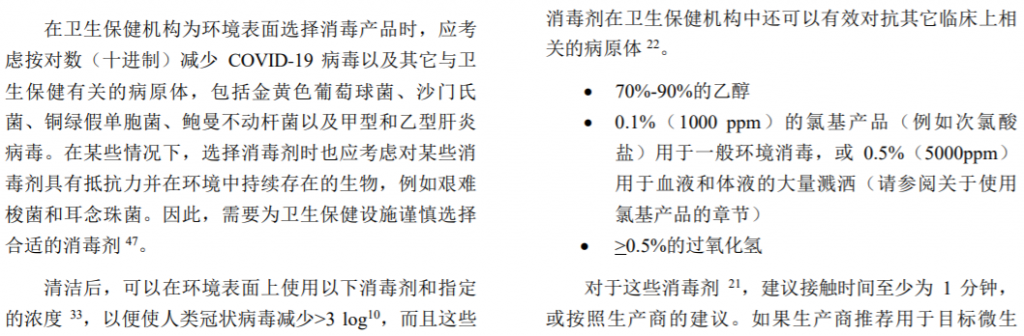
在执行某些医疗程序的卫生保健机构中,环境表面更有可能被COVID-19病毒污染6-8。因此,尤其在护理COVID-19患者的地方,必须妥善地对这些表面进行清洁和消毒以防止进一步传播。同样,此建议适用于无并发症且病情较轻的COVID-19患者的其它隔离环境,包括家庭和非传统设施9。
COVID-19病毒的传播与封闭环境中的人际密切接 触有关,例如在家庭、卫生设施、辅助生活和居住机构 等环境中10。此外,己发现卫生保健机构以外的社区环 境容易出现COVID-19传播事件,包括在公共建筑物、世卫组织当前针对非卫生保健机构环境的临时指导文件(包 括环境清洁和消毒建议)的主题,包括宗教团体机构12、丧葬服务13、工作场所14、食品部门15、住宿部门16、航空业17、 海事部门18、学校19、监狱和其它拘留场所20。
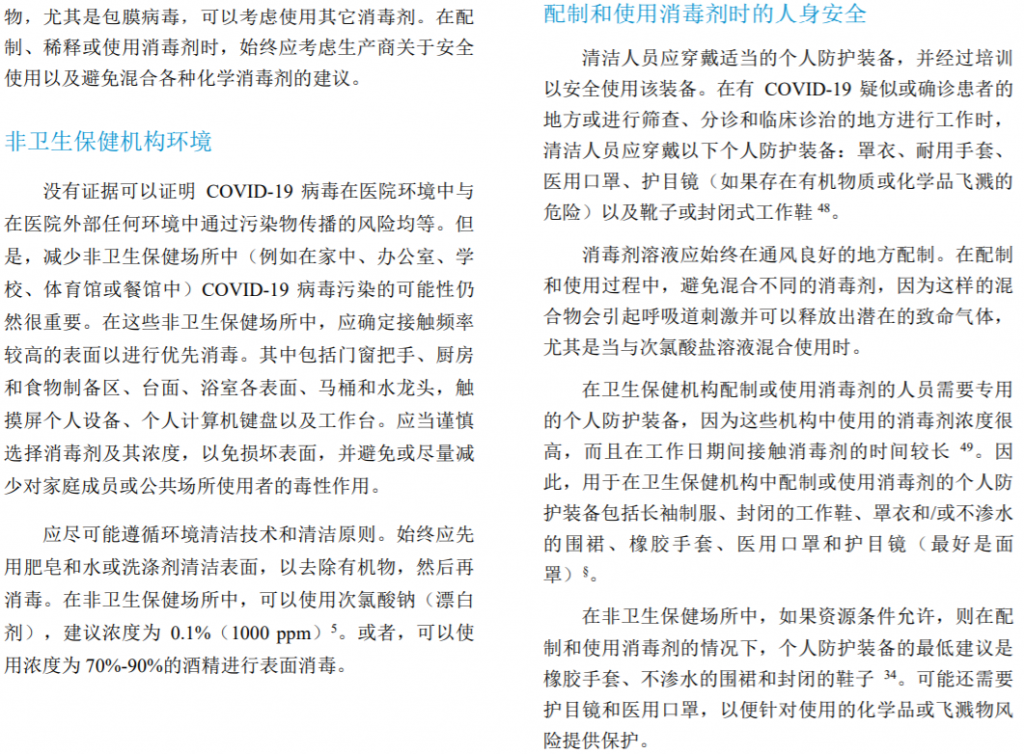
宗教团体中心、市场、交通和商业环境中10,11。尽管目 前尚不知道污染物传播的确切作用以及在卫生保健机构 之外进行消毒的必要性,但在本指导文件中对旨在减少 卫生保健机构中病原体传播的感染预防和控制原则(包 括清洁和消毒措施)做出了调整,以便可以将其应用于 非卫生保健机构的环境中*。在所有环境中,包括由于 资源有限而无法定期进行清洁和消毒的环境中,经常洗 手和避免触摸面部应该是减少与表面污染相关的任何潜 在传播的主要预防方法21。
与其它冠状病毒一样,SARS-CoV-2是一种包膜病 毒,具有脆弱的外部脂质包膜,与轮状病毒、诺如病毒 和脊灰病毒等非包膜病毒相比,它更容易受到消毒剂的 危害22。若干研究评估了 COVID-19病毒在不同表面上 的持久性。一项研究发现,COVID-19病毒在布和木料 上可存活1天,在玻璃上可存活2天,在不锈钢和塑料 上可存活4天,在医用口罩的外层可存活7天23。另一 项研究发现,COVID-19病毒在铜质物体上可存活4小 时,在纸板上可存活24小时,在塑料和不锈钢上可存活 72小时24。COVID-19病毒还可以在范围广泛的pH值和 环境温度下存活,但不能耐受高温和标准消毒方法23。 但是,这些研究是在没有采取清洁和消毒措施的实验室 条件下进行的,在实际环境中应谨慎解释。
本文件的目的是就COVID-19背景下对环境表面进 行清洁和消毒提供指导。
本指导文件适用于制定和实施COVID-19背景下对 环境表面进行清洁和消毒的政策和标准操作程序的卫生 保健专业人员,公共卫生专业人员和卫生主管当局。

参考文献
1.Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Geneva: World Health Organization; 2020 (https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations, accessed 6 May 2020)
2.Cheng, V.C.C., Wong, S.-C., Chen, J.H.K., Yip, C.C.Y., Chuang, V.W.M., Tsang, O.T.Y., et al, 2020. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 41, 493-498. (https://doi.org/10.1017/ice.2020.58, accessed 6 May 2020)
3.Lai, C.-C., Shih, T.-P., Ko, W.-C., Tang, H.-J., Hsueh, P.-R., 2020. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 55, 105924. (https://doi.org/10.1016/i.ijantimicag.2020.105924, accessed 6 May 2020)
4.Ramesh, N., Siddaiah, A., Joseph, B., 2020. Tackling corona virus disease 2019 (COVID 19) in workplaces. Indian J Occup Environ Med 24, 16. (https://doi.org/10.4103/ijoem.IJOEM 49 20, accessed 6 May 2020)
5.Bennett, J.E., Dolin, R., Blaser, M.J. (Eds.), 2015. Mandell, Douglas, and Bennetfs principles and practice of infectious
diseases,Eighthedition.ed.Elsevier/Saunders,Philadelphia,PA.
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7099662/, accessed 6 May 2020)
6.Ye, G., Lin, H., Chen, L., Wang, S., Zeng, Z., Wang, W., et al., 2020. Environmental contamination of the SARS-CoV-2 in healthcare premises: An urgent call for protection for healthcare workers (preprint). Infectious Diseases (except HIV/AIDS). (https://doi.org/10.1101/2020.03.11.20034546, accessed 6 May 2020)
7.Ong, S.W.X., Tan, Y.K., Chia, P.Y., Lee, T.H., Ng, O.T., Wong, M.S.Y., et al., 2020. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA 323, 1610. (https://doi.org/10.1001/jama.2020.3227, accessed 6 May 2020)
8.Faridi, S., Niazi, S., Sadeghi, K., Naddafi, K., Yavarian, J., Shamsipour, M., et al., 2020. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ 725, 138401. (https://doi.org/10.1016/j.scitotenv.2020.138401, accessed 6 May 2020)
9.Home care for patients with suspected novel coronavirus (nCoV) infection presenting with mild symptoms and management of contacts. Geneva: World Health Organization; 2020 (https://www.who.int/publications-detail/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts, accessed 10 May 2020)
10.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Geneva: World Health Organization; 2020 (https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf, accessed 10 May 2020)
11.Koh, D., 2020. Occupational risks for COVID-19 infection. Occup Med 70, 3-5. (https://doi.org/10.1093/occmed/kqaa036, accessed 10 May 2020)
12.Practical considerations and recommendations for Religious Leaders and Faith-based Communities in the context of COVID-19. Geneva: World Health Organization; 2020 (https://www.who.int/publications-detail/practical-considerations-and-recommendations-for-religious-leaders-and-faith-based-communities-in-the-context-of-covid-19, accessed 10 May 2020)
13.Infection prevention and control for the safe management of a dead body in the context of COVID-19: interim guidance. Geneva: World Health Organization; 2020 (https://www.who.int/publications-detail/infection-prevention-and-control-for-the-safe-management-of-a-dead-body-in-the-context-of-covid-19-interim-guidance, accessed 10 May 2020)
14.Getting your workplace ready for COVID-19: How COVID-19 spreads. Geneva; World Health Organization; 2020 (https://www.who.int/who-documents-detail/getting-your-workplace-ready-for-covid-19-how-covid-19-spreads)
15.COVID-19 and food safety: Guidance for food businesses. Geneva; World Health Organization; 2020
(https://apps.who.int/iris/bitstream/handle/10665/331705/WHO-2019-nCoV-Food_Safetv-2020.1-eng.pdf, accessed 10 May 2020)"
16.Operational considerations for COVID-19 management in the accommodation sector. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/bitstream/handle/10665/331937/WHO-2019-nCoV-Hotels-2020.2-eng.pdf, accessed 10 May 2020)
17.Operational considerations for managing COVID-19 cases or outbreak in aviation: interim guidance. Geneva; World Health Organization; 2020 (https://www.who.int/publications-detail/operational-considerations-for-managing-covid-19-cases-or-outbreak-in-aviation-interim-guidance, accessed 10 May 2020)
18.Operational considerations for managing COVID-19 cases or outbreaks on board ships: interim guidance. Geneva; World Health Organization; 2020 (https://www.who.int/publications-detail/operational-considerations-for-managing-covid-19-cases-or-outbreaks-on-board-ships-interim-guidance, accessed 10 May 2020)
19.Key Messages and Actions for COVID-19 Prevention and Control in Schools. Geneva; World Health Organization; 2020 (https://www.who.int/docs/default-source/coronaviruse/key-messages-and-actions-for-covid-19-prevention-and-control-in-schools-march-2020.pdf?sfvrsn=baf81d52_4, accessed 10 May 2020)
20.Preparedness, prevention and control of COVID-19 in prisons and other places of detention (http://www.euro.who.int/en/health-topics/health-determinants/prisons-and-health/publications/2020/preparedness,-prevention-and-control-of-covid-19-in-prisons-and-other-places-of-detention-2020, accessed 10 May 2020)
21.Risk Communication and Community Engagement (RCCE) Action Plan Guidance COVID-19 Preparedness and Response; Geneva: World Health Organization; 2020 (https://www.who.int/publications-detail/risk-communication-and-communitv-engagement-(rcce)-action-plan-guidance, accessed 14 May 2020)
22.Rutala, W.A., Weber, D.J., 2019. Best practices for disinfection of noncritical environmental surfaces and equipment in health care facilities: A bundle approach. Am J Infect Control 47, A96-A105. (https://doi.org/10.1016/j.ajic.2019.01.014, accessed 6 May 2020)
23.Chin, A.W.H., Chu, J.T.S., Perera, M.R.A., Hui, K.P.Y., Yen, H.-L., Chan, M.C.W., et al., 2020. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe S2666524720300033. (https://doi.org/10.1016/S2666-5247(20)30003-3, accessed 6 May 2020)
24.van Doremalen, N., Bushmaker, T., Morris, D.H., Holbrook, M.G., Gamble, A., Williamson, B.N., et al., 2020. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 382, 1564-1567. (https://doi.org/10.1056/NEJMc2004973, accessed 6 May 2020)
25. Essential environmental health standards in health care. Geneva:World Health Organization; (https://www.who.int/water sanitation health/publications/ehs hc/en/, accessed 6 May 2020)
26.CDC and ICAN. Best Practices for Environmental Cleaning in Healthcare Facilities in Resource-Limited Settings. Atlanta, GA: US Department of Health and Human Services, CDC; Cape Town, South Africa: Infection Control Africa Network; 2019. (https://www.cdc.gov/hai/pdfs/resource-limited/environmental-cleaning-RLS-H.pdf, accessed 6 May 2020)
27.Decontamination and Reprocessing of Medical Devices for Health-care Facilities. Geneva: World Health Organization; (https://www.who.int/infection-prevention/publications/decontamination/en/, accessed 6 May 2020)
28.Implementation manual to prevent and control the spread of carbapenem-resistant organisms at the national and health care facility level. Geneva: World Health Organization; 2019 (https://apps.who.int/iris/bitstream/handle/10665/312226/WHO-UHC-SDS-2019.6-eng.pdf, accessed 10 May 2020)
29.List N: Disinfectants for Use Against SARS-CoV-2 | US EPA. 2020. (https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2, accessed 6 May 2020)Rutala, W.A., Weber, D.J., 1997. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin. Microbiol. Rev. 10, 597-610. https://doi.org/10.1128/CMR.10.4.597, accessed 6 May 2020)
30.Pereira, S.S.P., Oliveira, H.M. de, Turrini, R.N.T., Lacerda, R.A., 2015. Disinfection with sodium hypochlorite in hospital environmental surfaces in the reduction of contamination and infection prevention: a systematic review. Rev. esc. enferm. USP 49, 0681-0688. (https://doi.org/10.1590/S0080-623420150000400020, accessed 6 May 2020)
31.Kohler, A.T., Rodloff, A.C., Labahn, M., Reinhardt, M., Truyen, U., Speck, S., 2018. Efficacy of sodium hypochlorite
against multidrug-resistant Gram-negative bacteria. J Hosp Infect 100,e40-e46。(https://doi.org/10.1016/j.jhin.2018.07.017, accessed 6 May 2020)
32.IL DIRETTORE GENERALE D'Amario, C. 2020. Disinfezione degli ambienti esterni e utilizzo di disinfettanti (ipoclorito di sodio) su superfici stradali e pavimentazione urbana per la prevenzione della trasmissione Dell'infezione da SARS-CoV-2. Minister。della Salute, (https://www.certifico.com/component/attachments/download/17156, accessed 6 May 2020)
33.Kampf, G., Todt, D., Pfaender, S., Steinmann, E., 2020. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104, 246-251. (https://doi.org/10.1016/i.ihin.2020.01.022, accessed 6 May 2020)
34.Yates, T., Allen, J., Leandre Joseph, M., Lantagne, D., 2017. WASH Interventions in Disease Outbreak Response. Oxfam; Feinstein International Center; UKAID. (https://doi.org/10.21201/2017.8753, accessed 6 May 2020)
35.Rutala, W.A., Cole, E.C., Thomann, C.A., Weber, D.J., 1998. Stability and Bactericidal Activity of Chlorine Solutions. Infect Control Hosp Epidemiol 19, 323-327. (https://doi.org/10.2307/30141372, accessed 6 May 2020)
36.Iqbal, Q., Lubeck-Schricker, M., Wells, E., Wolfe, M.K., Lantagne, D., 2016. Shelf-Life of Chlorine Solutions
Recommended in Ebola Virus Disease Response. PLoS ONE 11,e0156136.https://doi.org/10.1371/iournal.pone.0156136, accessed 6 May 2020)
37.Lantagne, D., Wolfe, M., Gallandat, K., Opryszko, M., 2018. Determining the Efficacy, Safety and Suitability of Disinfectants to Prevent Emerging Infectious Disease Transmission. Water 10, 1397. (https://doi.org/10.3390/w10101397, accessed 6 May 2020)
38.Roth, K., Michels, W., 2005. Inter-hospital trials to determine minimal cleaning performance according to the guideline by DGKH, DGSV and AKI 13, 106-110+112.
(https://www.researchgate.net/profile/Winfried_Michels/publication/292641729_Inter-
hospital_trials_to_determine_minimal_cleaning_performance_according_to_the_guideline_by_DGKH_DGSV_and_AKI /links/571a4d4108ae7f552a472e88/Inter-hospital-trials-to-determine-minimal-cleaning-performance-according-to-the-guideline-by-DGKH-DGSV-and-AKI.pdf, accessed 6 May 2020)
39.Mehtar, S., Bulabula, A.N.H., Nyandemoh, H., Jambawai, S., 2016. Deliberate exposure of humans to chlorine-the aftermath of Ebola in West Africa. Antimicrob Resist Infect Control 5, 45. (https://doi.org/10.1186/s13756-016-0144-1, accessed 6 May 2020)
40.Zock, J.-P., Plana, E., Jarvis, D., Anto, J.M., Kromhout, H., Kennedy, S.M., Kunzli, N., et al., 2007. The Use of Household Cleaning Sprays and Adult Asthma: An International Longitudinal Study. Am J Respir Crit Care Med 176, 735-741. (https://doi.org/10.1164/rccm.200612-1793OC, accessed 6 May 2020)
41.Schyllert, C., Ronmark, E., Andersson, M., Hedlund, U., Lundback, B., Hedman, L., et al., 2016. Occupational exposure to chemicals drives the increased risk of asthma and rhinitis observed for exposure to vapours, gas, dust and fumes: a crosssectional population-based study. Occup Environ Med 73, 663-669. (https://doi.org/10.1136/oemed-2016-103595, accessed 6 May 2020)
42.Weber, D.J., Rutala, W.A., Anderson, D.J., Chen, L.F., Sickbert-Bennett, E.E., Boyce, J.M., 2016. Effectiveness of ultraviolet devices and hydrogen peroxide systems for terminal room decontamination: Focus on clinical trials. Am J Infect Control 44, e77-e84. (https://doi.org/10.1016/j.aiic.2015.11.015, accessed 6 May 2020)
43.Marra, A.R., Schweizer, M.L., Edmond, M.B., 2018. No-Touch Disinfection Methods to Decrease Multidrug-Resistant Organism Infections: A Systematic Review and Meta-analysis. Infect. Control Hosp. Epidemiol. 39, 20-31. (https://doi.org/10.1017/ice.2017.226, accessed 6 May 2020)
44.Rutala, W.A., Weber, D.J., 2013. Disinfectants used for environmental disinfection and new room decontamination technology. Am J Infect Control 41, S36-S41. (https://doi.org/10.1016/i.aiic.2012.11.006, accessed 6 May 2020)
45.Benzoni, T., Hatcher, J.D., 2020. Bleach Toxicity, in: StatPearls. StatPearls Publishing, Treasure Island (FL). (https://www.ncbi.nlm.nih.gov/books/NBK441921/, accessed 6 May 2020)
46.Gon, G., Dancer, S., Dreibelbis, R., Graham, W.J., Kilpatrick, C., 2020. Reducing hand recontamination of healthcare workers during COVID-19. Infect. Control Hosp. Epidemiol. 1-2. (https://doi.org/10.1017/ice.2020.111, accessed 9 May 2020)
47.Water, sanitation, hygiene, and waste management for the COVID-19 virus. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC WASH-2020.3-eng.pdf, accessed 6 May 2020)
48.Rational use of personal protective equipment for coronavirus disease (COVID-19); Geneva: World Health Organization; 2020 (https://www.who.int/emergencies/diseases/novelcoronavirus-2019/technical-guidance/infectionprevention-and-control, accessed 6 May 2020)
49.Medina-Ramon, M., 2005. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case-control study. Occup Environ Med 62, 598-606. (https://doi.org/10.1136/oem.2004.017640, accessed 6 May 2020)
致谢
本文件是与以下各方协商后制定的:
Elizabeth Bancroft (美国疾病控制与预防中心);Gregory Built (联合国儿童基金会);Nizam Damani (英国贝尔法 斯特女王大学);Fernanda Lessa (美国疾病控制与预防中心);ShaheenMehtar (南非开普敦,斯泰伦博斯大学); Molly Patrick (美国疾病控制与预防中心);Mitchell Schwaber (以色列卫生部国家感染控制中心);Mark Sobsey (美国
北卡罗来纳州北卡罗来纳大学教堂山分校);以及David Weber (美国北卡罗来纳州北卡罗来纳大学教堂山分校);
世界卫生组织:
Benedetta Allegranzi, April Baller, Ana Boischio, Ana Paula Coutinho, Jennifer DeFrance, Jorge Durand, Bruce Allan Gordan, Rick Johnson, Margaret Montgomery, Carmen Lucia Pessoa da Silva, Madison Moon, Maria Clara Padoveze, Joanna Tempowski, Anthony Twyman, Maria Van Kerkhove, Bassim Zayed 和 Masahiro Zakoji。
世卫组织继续密切监测局势,以发现可能影响本临时指导文件的任何变化。如果任何因素发生变化,世卫组织将发 布一份更新。否则,本临时指导文件将在发布之日起两年后失效。
©世界卫生组织,2020年。保留部分版权。本作品可根据CC BY-NC-SA 3.0 IGO许可证获得。
世卫组织参考编号:WHO/2019-nCoV/Disinfection/2020.1